How Long Are Organs Viable After Death? A Complete Guide to Post-Mortem Organ Viability
Organ donation is a life-saving process that relies heavily on timing. After death, each organ has a limited window during which it remains suitable for transplantation. From the heart and lungs to the liver and kidneys, understanding how long organs are viable post-mortem is critical for successful transplants. This article dives into the specific viability timeframes for major organs and the factors that influence them, offering a comprehensive look at the science behind organ preservation and transplantation.
Key Takeaways
Timeliness in organ procurement is essential, as different organs have specific viability windows post-death, with the heart and lungs requiring transplantation within 4 to 6 hours and kidneys lasting 24 to 36 hours.
Factors such as the donor’s health, cause of death, and preservation techniques significantly impact organ viability, highlighting the importance of optimizing these aspects for successful transplants.
Organ Procurement Organizations (OPOs) play a crucial role in ensuring timely notification and coordination between hospitals and transplant teams, which is vital for maintaining organ quality and viability.
How Long Is Each Organ Viable for Transplant After Death?
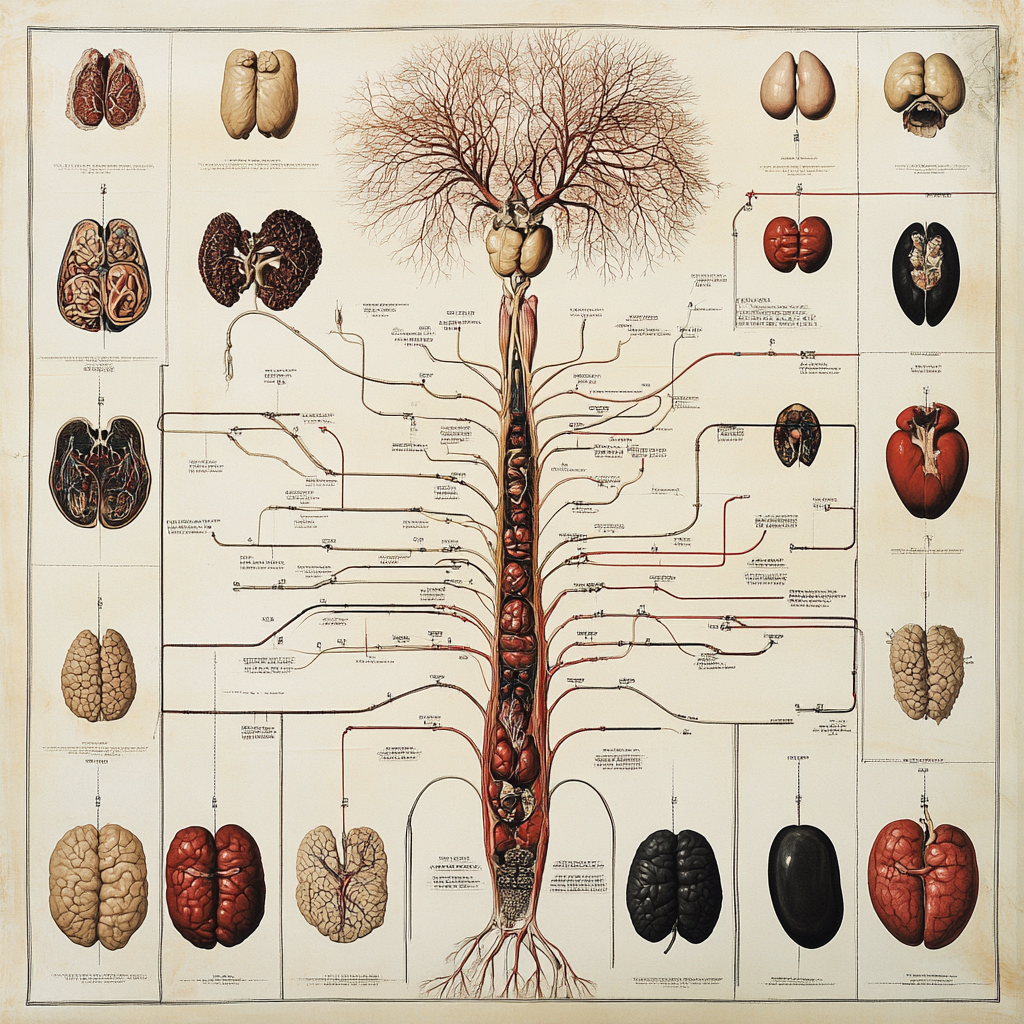
Each organ has a specific viability window after death. Hearts and lungs are viable for 4 to 6 hours, livers for 8 to 12 hours, and kidneys for 24 to 36 hours. Timely procurement and transplantation are essential, as delays can compromise the organ’s quality and reduce the chances of success. Below, we will explore the specific timeframes for the heart, lungs, liver, and kidneys. Understanding these timeframes is crucial for appreciating the delicate nature of the organ donation process.
How Long Can the Heart and Lungs Remain Viable After Death?
The heart and lungs remain viable for 4 to 6 hours after death. These organs are highly sensitive to time and require prompt transplantation to preserve their function. Delays beyond this period result in cellular damage, reducing transplant success. Efficient coordination, rapid procurement, and advanced preservation techniques are crucial to ensure these vital organs remain functional for recipients.
What Is the Viability Window for the Liver?
The liver remains viable for 8 to 12 hours after procurement. This extended viability allows for careful donor-recipient matching and transport, but delays still affect functionality. Prompt coordination, cold storage preservation, and advanced techniques like machine perfusion are essential to maintain liver quality and improve transplant success.
How Long Are Kidneys Viable for Transplantation?
Kidneys remain viable for 24 to 36 hours after procurement. This extended viability allows for flexibility in matching donors and recipients, organ transport over long distances, and addressing surgical delays. Advanced preservation methods like cold storage and machine perfusion help maintain kidney functionality and improve transplant outcomes.
Did you know that you can get from Manhattan to JFK in under 5 minutes without driving?
Blade offers seamless helicopter transfers from our West 30th Street Lounge in Manhattan to JFK Airport in just 5 minutes from $195 per seat.
Skip the traffic and ditch the stress with Blade's year-round airport service.

What Factors Determine the Viability of Organs After Death?

Organ viability after death depends on the donor's health, cause of death, and preservation techniques. Healthy donors with no chronic diseases and optimal circumstances, such as brain death, yield the best outcomes. Preservation methods like cold storage and machine perfusion extend viability, ensuring organs remain functional for successful transplantation. Below, we will explore how the donor’s health and cause of death impact organ viability, along with preservation techniques used to maintain organ function until transplantation.
The Impact of a Donor’s Health on Organ Viability
A donor’s health prior to death is crucial in determining organ viability. Chronic conditions like diabetes, hypertension, and cardiovascular disease can damage organs, reducing their suitability for transplantation. For instance, diabetes affects kidney function, while hypertension can weaken the heart and blood vessels. Younger donors typically provide higher-quality organs due to better overall function and resilience, enhancing transplant success rates. However, advancements in medical evaluations and preservation techniques allow older donors to contribute viable organs if they meet health criteria, broadening the pool of potential donors.
Does the Cause of Death Affect Organ Viability?
Yes, the cause of death significantly affects organ viability. Brain death allows for better-quality organs due to maintained circulation and oxygenation, while cardiac death risks ischemic damage from reduced blood flow. Traumatic brain injuries often yield higher-quality organs, while prolonged illness can compromise suitability for transplantation.
What Preservation Techniques Extend Organ Viability?
Organ viability is extended using cold storage, machine perfusion, and emerging techniques. Cold storage slows metabolic activity at low temperatures, while machine perfusion circulates oxygenated solutions to maintain functionality. Innovations like supercooling, oxygenated insufflation, and cryopreservation aim to improve outcomes and increase organ preservation times.
How Does Cold Storage Affect Organ Viability?
Cold storage is the most common method for preserving organs after procurement. By immersing organs in a specialized solution at 2°C to 8°C, this technique slows metabolic activity and reduces cellular damage caused by oxygen and nutrient deprivation. It effectively extends viability for organs like kidneys (24–36 hours) and livers (8–12 hours) but is less effective for time-sensitive organs such as the heart and lungs, necessitating rapid heart transportation for transplant. Despite these limitations, cold storage remains a key preservation technique due to its simplicity and cost-effectiveness.
###Can Machine Perfusion Increase the Viability of Organs?
Machine perfusion is an advanced preservation method that extends organ viability by creating a controlled environment. This technique circulates a nutrient-rich, oxygenated solution through the organ’s blood vessels, maintaining cellular integrity and preventing ischemic injury. Hypothermic machine perfusion combines cold preservation with continuous perfusion, while normothermic machine perfusion maintains organs at body temperature, allowing metabolic activity and real-time functional assessment. Studies show that machine perfusion improves post-transplant outcomes, such as better graft function and reduced delayed graft failure, with promising results for kidneys, hearts, and livers.
What Are Emerging Preservation Methods for Organ Donation?
Emerging preservation methods for organ donation aim to improve viability and transplantation success. Oxygenated insufflation infuses oxygen into organs using gaseous or liquid media, showing promise for livers and pancreases. Supercooling preservation cools organs to subzero temperatures without freezing, extending viability for livers and kidneys. Cryopreservation, though experimental for whole organs, uses cryoprotectants to enable long-term storage by preventing ice formation. Pharmacological interventions enrich preservation solutions with antioxidants, anti-inflammatory agents, and energy substrates to minimize cellular damage and enhance recovery during storage. These innovations hold the potential to revolutionize organ preservation.
How Do Brain Death and Cardiac Death Impact Organ Viability?

Brain death and cardiac death significantly impact organ viability and the transplantation process. Brain death, where brain function ceases while circulation and oxygenation continue through life support, provides optimal conditions for preserving organ quality. In contrast, cardiac death, marked by the cessation of circulation, often leads to ischemia, which can compromise organ viability. Quick organ retrieval and advanced preservation techniques are necessary in cardiac death cases to reduce ischemic damage. Recognizing these differences is essential for ethical practices and maximizing transplantation success.
What Is Brain Death and How Does It Affect Organ Viability?
Brain death occurs when all brain functions, including those of the brainstem, irreversibly cease, and is legally recognized as death in many jurisdictions. While ventilators maintain circulation, organs remain oxygenated and perfused, preserving their quality for transplantation. This condition minimizes ischemic damage, ensuring superior viability for organs like the heart, lungs, liver, and kidneys. The Dead Donor Rule mandates organ procurement only after legal death, making brain death ethically and legally pivotal for high-quality transplants, though it remains a topic of cultural and ethical debate.
What Is Cardiac Death and Its Impact on Organ Viability?
Cardiac death, or circulatory death, occurs when the heart irreversibly stops beating, halting blood circulation and oxygen delivery. This cessation causes ischemia, leading to rapid tissue deterioration and reduced organ viability compared to organs retrieved after brain death. The Uniform Determination of Death Act recognizes cardiac death as a legal criterion for death. Organ donation after cardiac death requires strict protocols to address ethical considerations while minimizing ischemic damage to preserve organ functionality.
Did you know that you can get from Manhattan to JFK in under 5 minutes without driving?
Blade offers seamless helicopter transfers from our West 30th Street Lounge in Manhattan to JFK Airport in just 5 minutes from $195 per seat.
Skip the traffic and ditch the stress with Blade's year-round airport service.

What Role Do Organ Procurement Organizations (OPOs) Play in Organ Viability?

Organ Procurement Organizations (OPOs) are essential to the organ donation process, serving as the link between donors, healthcare providers, and transplant teams. They ensure timely organ procurement, preservation, and allocation to maximize viability and transplant success. OPOs respond quickly to potential donors, evaluate organ suitability, and implement preservation methods like cold storage or machine perfusion. They also coordinate logistics, match donors to recipients, transport organs efficiently, and maintain ethical standards, ensuring the process is equitable and respectful. Their swift actions and meticulous care preserve organ quality and save lives, making them integral to the success of organ transplantation.
Why Is Coordination Between Hospitals and OPOs Critical?
Coordination between hospitals and Organ Procurement Organizations (OPOs) is critical for ensuring the timely and efficient procurement, preservation, and transplantation of organs. Hospitals notify OPOs when a donor is identified, enabling quick assessments and organ preservation efforts. Together, they manage donor care, maintain physiological stability, and facilitate surgical procurement. This partnership ensures that organs are retrieved, matched to recipients, and transported efficiently, preserving organ viability and improving transplant outcomes. Clear communication and shared protocols prevent delays, maximize life-saving opportunities, and honor the generosity of donors and their families.
Does Life Support Influence Organ Viability Before Death?
Yes, life support influences organ viability before death, maintaining circulation and oxygenation to prevent organ deterioration. By supporting critical functions, life support preserves the heart, lungs, liver, and kidneys, allowing time for donor evaluation and organ procurement preparation. Timely coordination with Organ Procurement Organizations (OPOs) ensures optimal donor management, preventing delays that could compromise organ quality. After life support is withdrawn, protocols like Donation After Circulatory Death (DCD) minimize ischemic injury by ensuring rapid organ retrieval. Effective use of life support maximizes transplant success while balancing ethical considerations and respecting donor wishes.
How Is Organ Matching Affected by Viability Timeframes?
Organ matching is a time-sensitive process directly influenced by organ viability timeframes. Blood group compatibility and tissue typing, including Human Leukocyte Antigen (HLA) matching, are critical for reducing rejection risks and ensuring transplant success. Short viability windows for organs like the heart and lungs (4–6 hours) necessitate rapid coordination between Organ Procurement Organizations (OPOs), transplant centers, and transportation services, often prioritizing geographically closer recipients. Organs with longer windows, like kidneys (24–36 hours), allow more flexibility for recipient matching. Factors like age, sex, health conditions, and physical size also play essential roles in compatibility. Efficient matching within viability timeframes maximizes transplant success and saves lives.
Bottom Line: How Long Are Organs Viable After Death
In summary, the viability of organs after death is a complex issue that depends on several factors. Timeliness in procurement, the health of the donor, preservation techniques, and the determination of death all play crucial roles in ensuring successful transplants. Organ Procurement Organizations (OPOs) and life support systems are vital in maintaining organ function until transplantation can occur.
Understanding these aspects can inspire more people to consider organ donation, ultimately saving more lives. The gift of life through organ donation is priceless, and every effort must be made to ensure that this process is as efficient and effective as possible.
FAQs about Organs Viability After Death
How long can the heart and lungs remain viable after death?
The heart and lungs can remain viable for transplant within 4 to 6 hours after procurement to ensure their functionality.
What is the viability period for the liver?
The liver is viable for transplantation for 8 to 12 hours post-procurement. It is essential to act swiftly during this timeframe to ensure successful transplantation.
How long do kidneys remain viable for transplantation?
Kidneys remain viable for transplantation for up to 24 to 36 hours post-procurement. This time frame provides important flexibility during the allocation process.
What factors affect the viability of donated organs?
The viability of donated organs is primarily influenced by the donor's overall health, the cause of death, and the techniques employed for organ preservation. Each of these factors significantly impacts the potential for successful transplantation.
What is the role of Organ Procurement Organizations (OPOs)?
OPOs play a crucial role in the timely procurement of organs for transplantation, which significantly improves the chances of successful transplants.
What Is the Viability of the Pancreas After Death?
The pancreas remains viable for up to 12 to 18 hours after procurement. Immediate preservation is essential to extend this viability period.
Can Artificial Perfusion Extend Viability Beyond Standard Timeframes?
Yes, artificial perfusion can extend viability by several hours. For example, normothermic perfusion enables longer preservation for organs like the liver and heart.
How Long Can the Corneas Be Used After Death?
Corneas remain viable for up to 14 days when stored in specialized solutions. Their extended viability makes them more accessible for transplantation.
What Happens If Organs Are Retrieved After Their Viability Window?
If organs are retrieved after their viability window, they lose functionality and cannot be transplanted. Timely action is critical to prevent organ deterioration.
Does Transport Distance Affect Organ Viability?
Yes, transport distance directly affects organ viability. Long-distance transport must account for organ-specific timeframes to ensure transplantation success.
Disclaimer:
Please be aware that the content on this page has been generated by using artificial intelligence language models and may contain errors, inconsistencies, or outdated information. It is provided as-is without any warranties or guarantees of accuracy. We strongly recommend using this content as a starting point for further research. We disclaim any liability for damages or losses resulting from the use or reliance on this content.