How Are Hearts Transported for Transplant: A Complete Guide
Transporting a donor heart for transplant is a delicate process that requires precision, speed, and advanced technology to ensure the organ remains viable. Hearts can deteriorate quickly once removed from the donor, making timely and efficient transportation crucial for a successful transplant. Whether through cold storage or cutting-edge perfusion systems, every step of the transport process is carefully coordinated to protect the heart and maximize its chances of functioning in the recipient’s body. This article explores how hearts are transported for transplant, the various preservation techniques used, and how innovations are improving the process to extend transport times and enhance outcomes.
Key Takeaways
The transportation of donor hearts is a complex process that relies on effective coordination, advanced preservation techniques, and optimized logistics to ensure successful transplantation.
Innovative systems such as the TransMedics Organ Care System (OCS) and the SherpaPak™ Cardiac Transport System enhance heart viability during transport by maintaining stability and enabling extended transport times.
Post-transplant care is vital for recipient health, with a focus on monitoring for rejection and adhering to medication regimens to support long-term success.
Why Is Heart Transportation Critical for Transplant Success?
Heart transportation is critical for transplant success due to the heart’s sensitivity to ischemic injury, requiring transplantation within 4 to 6 hours. Delays can cause tissue degradation, leading to complications or organ failure. Coordinated efforts by medical teams, OPOs, and transport specialists ensure fast, secure delivery, preserving heart viability and patient survival.
The Role of Timing in Donor Heart Viability
Timing directly affects donor heart viability because prolonged transport without oxygenated blood leads to tissue damage. Hearts must be transplanted within 4 hours to prevent ischemic injury. Shorter ischemic times increase transplant success, requiring seamless coordination between surgical teams, OPOs, and transport specialists to minimize delays.
Factors That Impact Heart Preservation During Transport
The preservation and health of a donor's heart during transport depend on temperature control, transport duration, handling, and logistics. Hearts must be kept at 4°C to 8°C to prevent ischemic injury, with cold storage limiting transit to 4 hours. Advanced systems like OCS extend viability to 8-10 hours by keeping the heart functioning.
How Is a Donor Heart Prepared for Transport?

A donor heart is prepared for transport by maintaining the donor’s physiological stability, carefully matching the heart to the recipient, and flushing it with cold preservation solution upon retrieval. The heart is placed in sterile, ice-filled containers to slow metabolism, ensuring viability for up to 4 hours during transit.
What Are the Key Steps in Donor Heart Retrieval?
Key steps in donor heart retrieval include maintaining donor life support, administering the cardioplegic solution to stop the heart, and carefully excising it to preserve vessels. The heart is flushed with preservation fluid and placed in sterile, ice-filled containers to prevent ischemic injury, ensuring viability for transplant.
How Is the Donor Heart Preserved Before Transport?
A donor's heart is preserved for organ transport using cold storage or advanced systems like TransMedics OCS. In cold storage, the heart is placed in sterile, ice-filled containers to slow metabolism, allowing for up to 4 hours of preservation. The OCS keeps the heart beating by perfusing it with oxygenated blood, extending viability to 8-10 hours.
How Does Traditional Cold Storage Preserve Hearts for Transplant?
Traditional cold storage preserves donor hearts by lowering the organ’s temperature to 4°C-8°C, slowing metabolic activity and reducing ischemic injury. The heart is flushed with preservation solution, triple-bagged, and surrounded by ice in a sterile container. This method extends viability for up to 4-6 hours during transport, ensuring transplant success.
What Are the Risks and Limitations of the Cold Storage Method for Heart Transplantation?
The main risks and limitations of cold storage for heart transplantation include hypothermic injury, a limited 4-6 hour preservation window, and the inability to monitor the heart during transport. Excessive cooling or delays can cause ischemic damage or freezing, reducing transplant success. Despite its simplicity and cost-effectiveness, cold storage restricts transport distances.
Did you know that you can get from Manhattan to JFK in under 5 minutes without driving?
Blade offers seamless helicopter transfers from our West 30th Street Lounge in Manhattan to JFK Airport in just 5 minutes from $195 per seat.
Skip the traffic and ditch the stress with Blade's year-round airport service.

What Are the Primary Transportation Options for Donor Heart Transplants?
The primary options used to transport organs for heart transplants include ground ambulances for local transfers, helicopters for regional transport, and fixed-wing aircraft or commercial flights for long-distance or international transplants. Ground and air transport ensure timely delivery, minimizing ischemic injury. Advanced preservation methods, like cold storage or perfusion systems, maintain heart viability during transit. The method chosen depends on distance, urgency, and available resources.
How Do Advanced Organ Care Systems Improve Heart Transport?
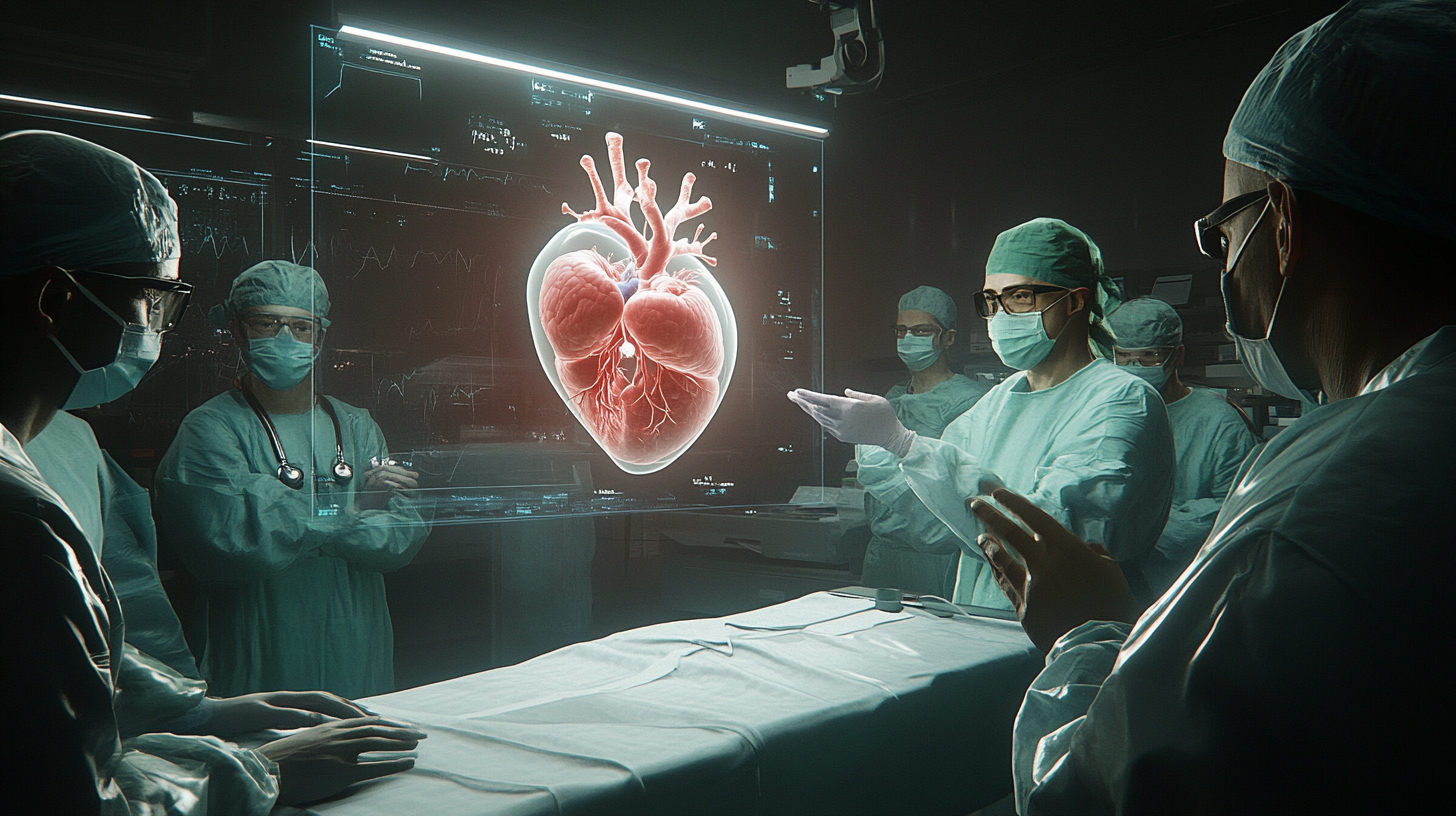
Advanced Organ Care Systems (OCS) improve heart transport by keeping the heart beating and perfused with oxygenated blood, reducing ischemic injury and extending preservation to 8-10 hours. Unlike cold storage, OCS allows real-time monitoring, expanding geographic transplant reach and improving success rates, particularly for donation after circulatory death (DCD) hearts.
Key Benefits of the Organ Care System (OCS) Over Traditional Methods
The Organ Care System (OCS) extends heart viability up to 10 hours, doubling the transport time of traditional cold storage. It allows long-distance organ procurement, expands donor options, and enables the use of marginal hearts through normothermic machine perfusion (NMP). The OCS provides real-time monitoring, improving transplant success and patient outcomes.
What is the Role of Perfusion Machines in Heart Transport?
Perfusion machines sustain donor hearts in a warm, beating state during transport by supplying oxygenated blood and nutrients, mimicking natural conditions. This reduces ischemic injury, extends heart viability up to 10 hours, and allows real-time monitoring. Unlike cold storage, perfusion machines enable the revival of marginal donor hearts, including those from circulatory death (DCD), expanding the donor pool. Continuous assessment during transport ensures optimal heart function, improving transplant success rates and reducing post-surgery complications like primary graft dysfunction (PGD). This innovation enhances organ availability and boosts long-term patient outcomes.
How Does the SherpaPak™ Cardiac Transport System Work?
The SherpaPak™ Cardiac Transport System preserves donor hearts by maintaining a stable temperature between 4°C and 8°C, preventing hypothermic injury. It uses phase change cooling and a sterile container to ensure aseptic conditions and protect the heart from contamination. Capable of preserving hearts for over 40 hours, SherpaPak™ extends transport time, enhances organ viability, and increases donor-recipient matching. This advanced system ensures consistent heart protection, improving transplant success rates.
Did you know that you can get from Manhattan to JFK in under 5 minutes without driving?
Blade offers seamless helicopter transfers from our West 30th Street Lounge in Manhattan to JFK Airport in just 5 minutes from $195 per seat.
Skip the traffic and ditch the stress with Blade's year-round airport service.

What Are the Main Challenges in Heart Transportation for Transplant?

The main challenges in heart transportation for transplants include limited preservation time (typically 4-6 hours), ischemic injury from cold storage, and logistical complexities during transit. Cold storage risks uneven cooling, leading to tissue damage or freezing injuries. Transport delays, weather, and lack of real-time monitoring can jeopardize organ viability. Advanced systems like the Organ Care System (OCS) and SherpaPak™ address these issues by extending preservation up to 10-40 hours, maintaining stable conditions, and enabling real-time organ assessment. This enhances organ viability, expands donor-recipient matching, and improves transplant success rates.
Does Real-time Monitoring Enhance Heart Viability During Transport?
Yes, real-time monitoring enhances heart viability during transport by continuously tracking temperature, blood flow, and organ health, ensuring the heart remains in optimal condition. Systems like TransMedics OCS and SherpaPak™ provide live feedback on critical metrics, allowing immediate corrections to prevent ischemic injury or hypothermic damage. This reduces the risk of primary graft dysfunction (PGD) and improves transplant success rates. Real-time monitoring also enables better coordination between transport teams and surgical staff, minimizing delays and increasing the likelihood of successful heart transplants by preserving organ integrity over longer distances.
What Is the Future of Heart Transport for Transplantation?
The future of heart transport for transplantation will be driven by advancements in normothermic perfusion, AI-driven monitoring, and extended preservation technologies. Systems like the TransMedics OCS increase preservation time to 8-10 hours, enabling long-distance transport. Smart transport containers and artificial blood substitutes will enhance organ viability, while dedicated air corridors and preservation hubs expand donor reach. These innovations aim to reduce organ wastage, increase transplant success, and improve global access to donor hearts.
Bottom Line: How are Hearts Transported for Transplant
The journey of a donor's heart from procurement to post-transplant care is a complex and highly coordinated process. Advancements in heart transportation techniques, such as the TransMedics Organ Care System and SherpaPak™ Cardiac Transport System, have significantly improved the viability and outcomes of heart transplants. These innovations address the limitations of traditional cold storage methods, providing stable environments and continuous monitoring to ensure the best possible condition of the donor's heart upon arrival at the transplant center.
As we continue to explore and implement new technologies in heart transplantation, the future looks promising for patients suffering from end-stage heart failure. The dedication and expertise of transplant teams, combined with state-of-the-art techniques, offer hope and a new lease on life for countless individuals. The ongoing advancements in heart transport promise to enhance the success rates and overall quality of heart transplants, paving the way for a brighter future in cardiac surgery.
FAQs about Heart Transportation for Transplant
What Methods Are Used to Transport Donor Hearts for Transplant?
Donor hearts are typically transported via ambulances, helicopters, fixed-wing aircraft, or commercial flights. The method chosen depends on distance, urgency, and available resources.
How Is a Donor Heart Kept Sterile During Transport?
To ensure sterility during transport, the heart is placed in a triple-layer sterile bag filled with preservation solution, which is then sealed in a sterile, ice-filled container. This multi-layer process protects the heart from contamination.
How Long Can a Donor Heart Remain Outside the Body During Transport?
A donor heart can remain outside the body for up to 4 hours with cold storage and 8-10 hours using perfusion systems like the TransMedics OCS. The heart must be transplanted within these timeframes to ensure viability.
Why Is Temperature Monitoring Critical During Heart Transport?
Temperature monitoring is critical during heart transport because maintaining the heart between 4°C and 8°C prevents tissue damage. If the temperature drops too low, freezing can occur, compromising the heart’s viability.
How Are Hearts Transported Across International Borders for Transplant?
Donor hearts can be transported across international borders using chartered flights or medical jets. Coordination between international OPOs and transplant centers ensures compliance with regulations and minimizes delays.
What Happens if a Donor Heart Is Delayed During Transport?
If a donor heart is delayed during transport, its viability may decrease, leading to potential ischemic injury. Perfusion systems like OCS can mitigate damage by keeping the heart oxygenated and beating longer than cold storage methods.
How Do Surgeons Determine if a Heart Is Still Viable After Transport?
Surgeons assess a heart’s viability by checking for adequate function, color, and structural integrity. In cases of perfusion transport, continuous monitoring allows surgeons to evaluate performance throughout the journey.
What Role Do Organ Procurement Organizations (OPOs) Play in Heart Transport?
OPOs coordinate the retrieval, preservation, and transportation of donor hearts, ensuring they reach recipients quickly and safely. They manage logistics and handle communication between donor and recipient hospitals.
How Does Air Transport Improve Heart Transplant Success Rates?
Air transport improves heart transplant success rates by reducing ischemic time, allowing hearts to be transported quickly over long distances. Helicopters and jets bypass traffic and provide direct hospital-to-hospital delivery.
What Specialized Equipment Is Used to Transport Hearts for Transplant?
Specialized equipment includes sterile containers, temperature-controlled transport boxes, and perfusion machines like the OCS, which keeps the heart beating and perfused during long-distance transport.
How Are Marginal Donor Hearts Transported Safely?
Marginal donor hearts are transported using perfusion machines that restore circulation and improve heart condition during transit. This allows surgeons to reassess viability upon arrival.
Can Multiple Organs Be Transported Together During Heart Transplants?
Yes, multiple organs from the same donor, such as lungs, kidneys, and livers, can be transported simultaneously. Each organ is packed separately in sterile containers to ensure individual preservation.
How Is the Transport of a Donor Heart Coordinated Between Teams?
Transport coordination involves real-time communication between the retrieval team, OPO, and transplant center. A dedicated transport team ensures the heart arrives at the recipient hospital promptly.
What Precautions Are Taken to Prevent Organ Damage During Transport?
To prevent damage, donor hearts are carefully packaged, monitored for temperature, and transported using direct, expedited routes. Perfusion systems further reduce the risk of ischemic injury.
How Do Organ Care Systems Reduce the Risk of Primary Graft Dysfunction (PGD)?
Organ Care Systems (OCS) reduce the risk of PGD by keeping the heart oxygenated and functional during transport, ensuring it arrives in optimal condition for transplant.
Disclaimer:
Please be aware that the content on this page has been generated by using artificial intelligence language models and may contain errors, inconsistencies, or outdated information. It is provided as-is without any warranties or guarantees of accuracy. We strongly recommend using this content as a starting point for further research. We disclaim any liability for damages or losses resulting from the use or reliance on this content.