How Air Pressure Affects Organ Viability: Impacts and Innovations
Air pressure is a critical factor in organ viability, particularly for organ transplants. It influences the preservation and functionality of organs by regulating cellular metabolism, blood flow, and oxygen delivery. This article explores how air pressure affects organ viability through different management techniques, focusing on methods like Hypothermic and Normothermic Machine Perfusion. Discover how optimizing air pressure can improve organ preservation and enhance transplant success rates.
Key Takeaways
Air pressure is crucial for organ preservation and transportation, significantly influencing cellular metabolism and blood flow in donor organs.
Innovative techniques such as Hypothermic Machine Perfusion (HMP) and Normothermic Machine Perfusion (NMP) utilize air pressure to enhance organ viability and improve transplant outcomes.
Research into advanced air pressure management methods and ethical considerations in organ donation is essential for optimizing strategies in organ preservation and ensuring patient safety.
The Role of Air Pressure in Organ Preservation

The role of air pressure in organ preservation is both profound and multifaceted. At its core, the right atmospheric pressure optimizes conditions that support cellular metabolism and blood flow in human organs. This delicate balance keeps donor organs viable for transplantation, improving clinical outcomes and increasing the availability of high-quality organs.
Organ perfusion, a key process in preserving organs, relies heavily on regulated air pressure. This includes the delivery of oxygen to tissues, which is crucial for maintaining metabolic activity and preventing damage during preservation. For instance, oxygenated machine perfusion is particularly significant for organs from donors after cardiac death, as it helps counteract warm ischemic injury, thereby enhancing organ quality. This technique underscores the importance of air pressure in facilitating effective organ preservation.
Cold preservation, involving temperatures between 5°C–8°C, can significantly enhance organ storage time, reducing the risk of damage. Controlled air pressure within these temperature ranges optimizes preservation techniques to maintain organ integrity over extended periods. This is especially critical for vital organs like the kidneys, liver, and lungs, which are highly susceptible to ischemic damage if not properly preserved.
In the realm of organ transplantation, the arterial pressure within the preservation systems plays a pivotal role. It ensures that perfusion solutions are uniformly distributed throughout the organ, enhancing microvascular blood flow and reducing the risk of cell damage. Careful regulation of air pressure preserves organs and improves transplant success rates.
The integration of advanced air pressure management techniques promises to revolutionize organ preservation and transplantation, providing hope for countless patients.
Mechanisms of Air Pressure Regulation in Organ Transport Systems
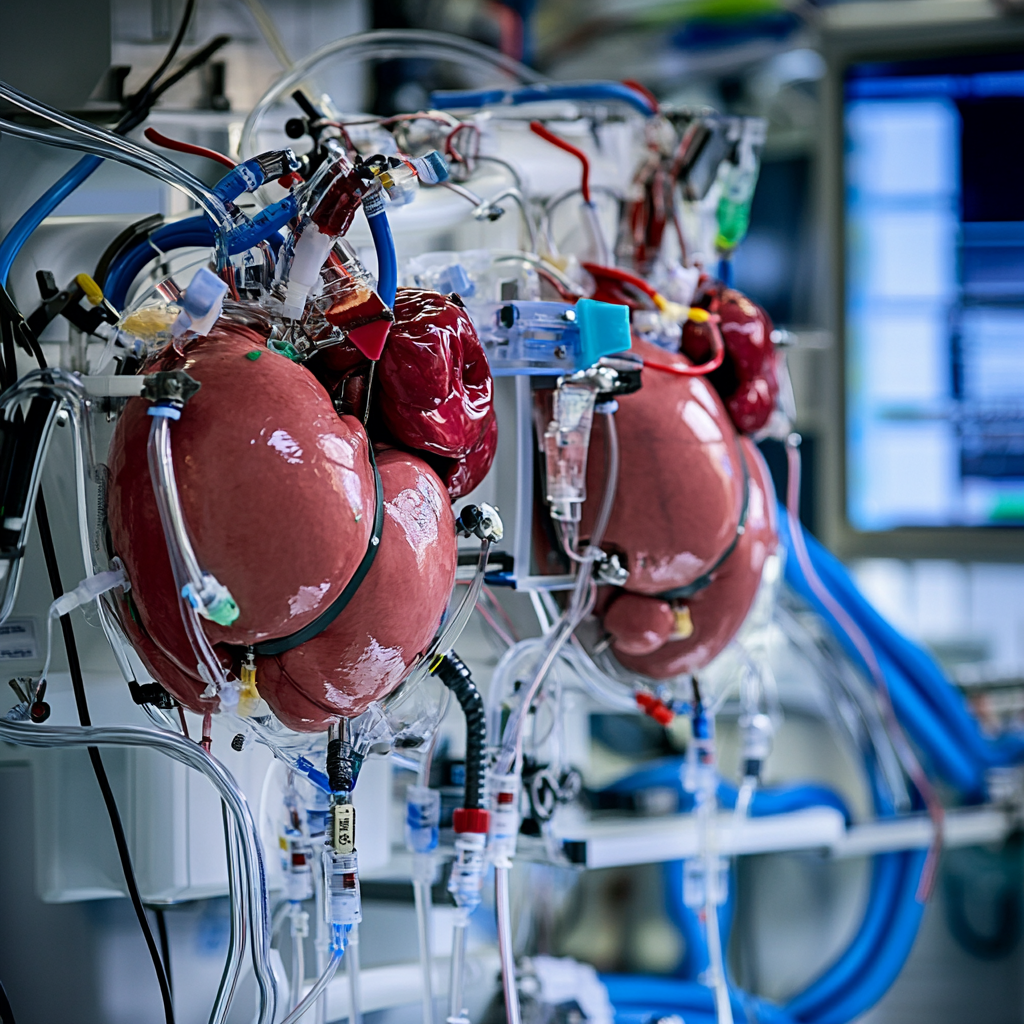
Modern organ transport systems have evolved to incorporate sophisticated mechanisms for regulating air pressure, ensuring that organs remain viable throughout the journey from donor to recipient. Controlled air pressure is fundamental to these systems, enhancing organ preservation and minimizing ischemic damage. This section will explore two primary methods of air pressure regulation: Hypothermic Machine Perfusion (HMP) and Normothermic Machine Perfusion (NMP).
The delivery of oxygen to tissues during preservation is a critical factor that air pressure regulation addresses. Maintaining optimal pressure levels sustains metabolic activity, prevents tissue trauma, and ensures effective organ perfusion. Variation in air pressure significantly impacts organ viability, influencing ATP levels and microvascular blood flow, essential for maintaining organ function during preservation.
Intermittent pressurization during kidney perfusion, for example, has been shown to enhance circulatory distribution and reduce cell damage. Stable air pressure during lung transport prevents tissue trauma and ensures organ viability. As we delve deeper into the specific mechanisms of HMP and NMP, we will see how these techniques leverage air pressure to optimize organ preservation.
Hypothermic Machine Perfusion (HMP)
Hypothermic Machine Perfusion (HMP) has significantly improved the outcomes of kidney transplants by providing a controlled environment that lowers metabolic rates and decreases cellular metabolic needs. Operating within a temperature range of 4°C–10°C, HMP uses air pressure to assist in the distribution of perfusing solutions, ensuring uniform circulation throughout the organ.
However, HMP is not without its drawbacks. Excessive damage to vascular endothelium, inadequate oxygen solubility, removal of protective substrates, organ edema, and increased cost are some of the challenges associated with this preservation technique. Despite these disadvantages, HMP’s ability to significantly enhance kidney perfusion and reduce ischemic injury duration makes it a valuable tool in organ preservation.
Air pressure in HMP is critical for maintaining optimal conditions for organ viability. Carefully regulated pressure levels in HMP minimize the risk of ischemia-reperfusion injury and improve the overall quality of the preserved organ. This technique exemplifies how advanced air pressure management can lead to better outcomes in organ transplantation, paving the way for further innovations in the field.
Normothermic Machine Perfusion (NMP)
Normothermic Machine Perfusion (NMP) represents a leap forward in organ preservation by mimicking physiological conditions to optimize organ viability. This technique supports cellular metabolism by delivering oxygen and nutrients while eliminating waste, thereby maintaining the organ in a near-living state. Balancing perfusion pressure and internal chamber pressure is vital for optimizing organ viability during NMP.
One of the significant advantages of NMP is its ability to facilitate real-time assessment of organ viability. This feature enhances decision-making regarding transplantation, allowing for better matching of donor organs to recipients and improving overall transplant success rates. Leveraging air pressure to mimic the body’s natural conditions, NMP offers a promising alternative to traditional preservation methods.
NMP’s ability to maintain organ function more effectively than static cold storage makes it a valuable tool in the quest to improve transplant outcomes. Further advancements in this technique will enhance the preservation and viability of a wide range of organs, ultimately saving more lives.
Did you know that you can get from Manhattan to JFK in under 5 minutes without driving?
Blade offers seamless helicopter transfers from our West 30th Street Lounge in Manhattan to JFK Airport in just 5 minutes from $195 per seat.
Skip the traffic and ditch the stress with Blade's year-round airport service.

Effects of Air Pressure on Different Organs
Air pressure plays a crucial role in maintaining the viability of different organs during preservation. Whether it’s the heart, liver, kidneys, or lungs, each organ has specific requirements for optimal preservation, and understanding air pressure dynamics is essential for improving preservation methods and enhancing transplant outcomes.
Techniques such as persufflation, which involve controlled air pressure, can benefit various organs, ensuring they remain viable for transplantation. The BAROguard system, for instance, is designed to examine the effects of maintaining consistent air pressure during the transport of organs, highlighting the importance of this factor in successful organ preservation.
The following subsections explore how air pressure affects kidney, liver, and lung preservation, each with unique challenges and solutions.
Kidney Preservation
Kidney preservation is particularly sensitive to air pressure dynamics. Increased interstitial pressure around capillaries from external pressurization can enhance microvascular blood flow, which is crucial for maintaining kidney function during preservation. Optimizing perfusion pressure between 80-120 mmHg has been shown to improve kidney filtration, enhancing the overall success of the preservation process.
During A-PSF (Aortic Perfusion with Sustained Flow), pressure levels of 90–100 mmHg are used effectively for kidney preservation, maintaining ATP levels crucial for kidney function post-transplant. However, challenges such as the deterioration of renal function after reperfusion in kidneys preserved under A-PSF highlight the need for continuous improvement in preservation techniques.
Hypothermic Machine Perfusion (HMP) has significantly enhanced the success rates of kidney transplants by reducing the duration of ischemic injury. Despite some disadvantages, HMP’s ability to maintain optimal conditions through regulated air pressure makes it a valuable tool in kidney preservation. The continuous refinement of these techniques promises better outcomes for kidney transplantation, providing hope for patients suffering from acute kidney injury and other renal conditions.
Liver Preservation
Liver preservation also benefits significantly from controlled air pressure. Maintaining adequate blood flow pressure during organ perfusion reduces the risk of ischemia-reperfusion injury, a common challenge in liver transplants. Techniques like Normothermic Machine Perfusion (NMP) replicate physiological conditions, allowing for better maintenance of liver function compared to traditional storage methods.
External pressure mitigates leakage of perfusing solutions from compromised vascular structures, ensuring liver viability for transplantation. This approach minimizes ischemic damage, improving the overall quality of the preserved liver and increasing the chances of successful transplantation outcomes.
As research continues to advance, new methods and technologies promise to further enhance liver preservation, providing better solutions for patients in need of liver transplantation.
Lung Preservation
Lung preservation presents unique challenges that can be addressed through controlled air pressure. In ex vivo lung perfusion, maintaining optimal air pressure is crucial for improving oxygen concentration and preventing cell edema. External air pressure during organ perfusion prevents the breakdown of vascular structures, ensuring lung viability for transplantation.
Pressure variations during the transport of donor lungs can cause tissue trauma, impacting lung viability. To address this, techniques like ex vivo lung perfusion have been developed to provide a controlled environment for assessing and repairing marginal donor organs before transplantation. This approach not only enhances lung preservation but also expands the donor pool, offering new hope for patients awaiting lung transplants.
The demand for marginal donor organs has spurred research into innovative preservation techniques, emphasizing the importance of air pressure management in improving transplant outcomes. As we continue to refine these methods, we can expect significant advancements in lung preservation, ultimately saving more lives and improving the quality of life for transplant recipients.
Innovations in Air Pressure Management for Organ Transplants
The field of organ transplantation is witnessing remarkable innovations in air pressure management, promising to enhance organ preservation and improve transplant outcomes. New strategies, like advanced machine perfusion techniques, aim to extend storage times and maintain organ viability through better air pressure regulation. These advancements address the limitations of traditional preservation methods and expand the donor pool.
Partial freezing, for example, has the potential to extend organ storage duration from weeks to months, significantly improving preservation outcomes. The BAROguard system leverages hypothermic preservation techniques while actively controlling airway pressure, enhancing lung transport viability. Such innovations demonstrate the potential of air pressure management in revolutionizing organ transplants and providing better solutions for patients in need.
Research into persufflation, which uses air pressure control to reduce edema formation and improve oxygenation, illustrates the benefits of advanced air pressure techniques. As we explore these innovations, we will see how they contribute to improving organ preservation and transplantation outcomes, offering new hope for patients worldwide.
External Pressure Dynamics
Optimal external pressure ensures effective kidney perfusion and overall organ viability. The new perfusion method, which applies an external pressure of 100 mmHg, enhances kidney perfusion by promoting consistent perfusate filtration through a steady supply of preservation solutions.
Machine perfusion techniques, being more dynamic and physiological, provide improved conditions for organ viability. By carefully regulating external pressure, these techniques help reduce blood vessel resistance and shear stress, preventing cell edema and ensuring that organs remain viable for transplantation. Additionally, they optimize the flow through blood vessels, enhancing nutrient delivery and waste removal.
The continuous refinement of external pressure dynamics promises to further enhance the success rates of organ transplants.
Controlled Rewarming Techniques
Controlled rewarming techniques are essential in improving graft preparation and increasing transplant success. One promising method, nanowarming, employs biocompatible iron oxide nanoparticles for uniform heating of vitrified organs, ensuring that they are rewarmed evenly and efficiently. This technique helps mitigate the risks associated with traditional rewarming methods, such as uneven heating and thermal stress, which can compromise organ viability.
Precise rewarming techniques enhance organ viability, making them crucial for successful transplants. These methods ensure organs reach physiological temperatures in a controlled manner, reducing damage risk and improving overall quality. Refining these techniques promises significant improvements in transplant outcomes, providing better solutions for patients.
In addition to nanowarming, other controlled rewarming techniques are being explored to further enhance organ preservation. These methods, often tested in randomized clinical trials, have shown promising results in maintaining organ function and viability during the rewarming process. As research progresses, integrating these techniques into standard preservation protocols promises to revolutionize organ transplantation.
Challenges and Future Directions

While air pressure regulation is critical for organ preservation, it faces significant challenges. One of the primary limitations is the static cold storage method, which, despite its widespread use, does not provide optimal conditions for organ viability. Extended ex vivo machine perfusion times facilitate organ repair and improve transplantation outcomes, highlighting current challenges in preserving organ viability.
The lack of detailed comparative studies poses challenges when selecting efficient perfusion modalities for organ preservation. This gap in research makes it difficult to determine the best practices for maintaining organ viability, highlighting the need for further studies and innovation in this field. Additionally, the exploration of acellular perfusates as alternatives to blood-based solutions in organ preservation is an emerging area of research that holds promise for future advancements.
Future strategies may include organ immunomodulation techniques to reduce rejection risks during ex vivo perfusion, enhancing the success rates of transplants. Emerging techniques like advanced perfusion, subzero, or isochoric preservation methods are potential future directions for improving organ viability. As research continues to evolve, these innovations promise to overcome current challenges and pave the way for better clinical outcomes in organ transplantation.
Did you know that you can get from Manhattan to JFK in under 5 minutes without driving?
Blade offers seamless helicopter transfers from our West 30th Street Lounge in Manhattan to JFK Airport in just 5 minutes from $195 per seat.
Skip the traffic and ditch the stress with Blade's year-round airport service.

Ethical Considerations in Organ Preservation Research
Ethical considerations are paramount in organ preservation research. Ethical guidelines in organ donation emphasize the importance of altruism and the principle of beneficence in medical practice. Explicit consent laws require individuals to proactively express their willingness to donate a donor organ, ensuring transparency and respect for donors’ wishes.
Presumed consent, which allows organ removal from deceased individuals unless they explicitly opted out during their lifetime, raises important ethical questions regarding autonomy and consent. Financial incentives for organ donation can further complicate the ethical landscape, leading to concerns about coercion and the commodification of human body parts. Ethics committees play a crucial role in overseeing potential conflicts of interest in organ donation to ensure fairness and transparency.
The ethical principle of non-maleficence is particularly relevant in organ transplants, especially concerning the risks to living donors. Future innovations in organ preservation may focus on optimizing preservation solutions and developing new therapeutic additives to promote cellular metabolism and viability. As we advance in this field, maintaining a strong ethical framework will be essential to ensure that the benefits of organ preservation research are realized without compromising ethical standards.
Bottom Line: How Air Pressure Affects Organ Viability: Impacts and Innovations
In summary, air pressure plays a critical role in organ preservation, influencing everything from cellular metabolism to blood flow and the overall quality of donor organs. Techniques like Hypothermic Machine Perfusion (HMP) and Normothermic Machine Perfusion (NMP) leverage air pressure to optimize organ viability, significantly improving transplant outcomes.
Understanding the effects of air pressure on different organs, such as the kidneys, liver, and lungs, is essential for developing effective preservation methods. Innovations in air pressure management, including external pressure dynamics and controlled rewarming techniques, promise to revolutionize the field of organ transplantation, offering new hope for patients in need.
As we continue to face challenges in air pressure regulation, ongoing research and innovation will be critical in overcoming these obstacles and improving clinical outcomes. By maintaining a strong ethical framework, we can ensure that advancements in organ preservation benefit patients while upholding the highest ethical standards. The future of organ transplantation is bright, with air pressure management playing a pivotal role in saving more lives and improving the quality of life for transplant recipients.
FAQs about How Air Pressure Affects Organ Viability
Why is air pressure important in organ preservation?
Air pressure is essential in organ preservation because it maintains optimal conditions for cellular metabolism and blood flow, thereby ensuring the viability of donor organs. Proper pressure levels contribute directly to the success of transplantation outcomes.
What are the main techniques used for air pressure regulation in organ transport systems?
The primary techniques for air pressure regulation in organ transport systems are Hypothermic Machine Perfusion (HMP) and Normothermic Machine Perfusion (NMP), both of which enhance organ viability and transplant outcomes. These methods utilize controlled air pressure to maintain optimal conditions during transportation.
How does air pressure affect kidney preservation?
Air pressure plays a crucial role in kidney preservation by improving microvascular blood flow and maintaining ATP levels, which reduces ischemic injury. This optimization ultimately leads to increased success rates in kidney transplants.
What are the ethical considerations in organ preservation research?
Ethical considerations in organ preservation research prominently feature the need for informed consent, the avoidance of financial coercion, transparency, and adherence to the principles of beneficence and non-maleficence. These aspects are crucial to uphold the integrity of the research and protect the rights of all involved parties.
What future directions are being explored in air pressure management for organ transplants?
Future directions in air pressure management for organ transplants focus on advanced perfusion techniques, subzero preservation, isochoric preservation, and organ immunomodulation to enhance clinical outcomes and minimize rejection risks. These innovations aim to significantly improve transplant viability and success rates.
Disclaimer:
Please be aware that the content on this page has been generated by using artificial intelligence language models and may contain errors, inconsistencies, or outdated information. It is provided as-is without any warranties or guarantees of accuracy. We strongly recommend using this content as a starting point for further research. We disclaim any liability for damages or losses resulting from the use or reliance on this content.